Stable angina is chest pain or discomfort that most often occurs with activity or emotional stress. Angina is due to poor blood flow through the blood vessels in the heart called the coronary arteries.
Causes
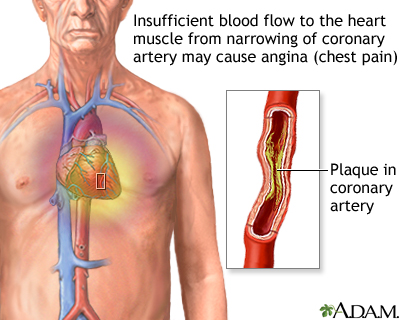
Your heart muscle needs a constant supply of oxygen. The coronary arteries carry oxygen-rich blood to the heart.
When the heart muscle has to work harder, it needs more oxygen. Symptoms of angina may occur when blood supply to the heart muscle is reduced. This happens when the coronary arteries are narrowed or blocked by atherosclerosis or by a blood clot.
The most common cause of angina is coronary artery disease. Angina pectoris is the medical term for this type of chest pain.
Stable angina is less serious than unstable angina, but it can be very painful or uncomfortable.
There are many risk factors for coronary artery disease. Some include:
- Diabetes
- Family history of early coronary heart disease (a close relative such as a sibling or parent had heart disease before age 55 in a man or before age 65 in a woman)
- High blood pressure
- High LDL cholesterol
- Low HDL cholesterol
- Obesity
- Sedentary lifestyle
- Smoking
- Advancing age
- Male sex
Anything that makes the heart muscle need more oxygen or reduces the amount of oxygen it receives can cause an angina attack in someone with heart disease, including:
- Cold weather
- Exercise
- Emotional stress
- Large meals
Other causes of angina include:
- Abnormal heart rhythms (your heart beats very quickly or your heart rhythm is not regular)
- Anemia
- Coronary artery spasm (also called Prinzmetal angina)
- Heart failure
- Heart valve disease
- Hyperthyroidism (overactive thyroid)
- Other uncommon abnormalities of the small branches of the coronary arteries or how the walls function (endothelial dysfunction)
Symptoms
Symptoms of stable angina are most often predictable. This means that about the same amount of exercise or activity may cause your angina to occur. Your angina should improve or go away quickly when you stop or slow down the exercise.
The most common symptom is chest pain that occurs behind the breastbone or slightly to the left of it. The pain of stable angina most often begins slowly and gets worse over the next few minutes before going away when the activity stops.
Typically, the chest pain feels like tightness, heavy pressure, squeezing, or a crushing feeling. It may spread to the:
- Arm (most often the left)
- Back
- Jaw
- Neck
- Shoulder
Some people say the pain feels like gas or indigestion.
Less common symptoms of angina may include:
- Fatigue
- Shortness of breath
- Weakness
- Dizziness or lightheadedness
- Nausea, vomiting, and sweating
- Palpitations
Pain from stable angina:
- Most often comes on with activity or stress
- Lasts an average of 1 to 15 minutes
- Is relieved with rest or a medicine called nitroglycerin
Angina attacks can occur at any time during the day. Often, they occur between 6 a.m. and noon.
Exams and Tests
Your health care provider will examine you and check your blood pressure. Tests that may be done include:
- Coronary angiography
- Blood cholesterol profile
- Electrocardiogram (ECG)
- Exercise tolerance test (stress test or treadmill test)
- Nuclear medicine (thallium) stress test
- Stress echocardiogram
- Heart CT scan
Treatment
Treatment for angina may include:
- Lifestyle changes
- Medicines
- Procedures such as coronary angioplasty with stent placement
- Coronary artery bypass surgery
If you have angina, you and your provider will develop a treatment plan. This plan should include:
- Medicines you regularly take to prevent angina
- Activities that you can do and those you should avoid
- Medicines you should take when you have angina pain
- Signs that mean your angina is getting worse
- When you should call your provider or get emergency medical help
MEDICINES
You may need to take one or more medicines to treat blood pressure, diabetes, or high cholesterol levels. Follow your provider's directions closely to help prevent your angina from getting worse.
Nitroglycerin pills or spray may be used to stop chest pain.
Anti-clotting medicines such as aspirin and clopidogrel (Plavix), ticagrelor (Brilinta) or prasugrel (Effient) can help prevent blood clots from forming in your arteries and reduce the risk of heart attack. Ask your provider if you should be taking these medicines.
You may need to take more medicines to help prevent you from having angina. These include:
- ACE inhibitors to lower blood pressure and protect your heart
- Beta-blockers to lower heart rate, blood pressure, and oxygen use by the heart
- Calcium channel blockers to relax arteries, lower blood pressure, and reduce strain on the heart
- Nitrates to help prevent angina
- Ranolazine (Ranexa) to treat chronic angina
NEVER STOP TAKING ANY OF THESE MEDICINES ON YOUR OWN. Always talk to your provider first. Stopping these medicines suddenly can make your angina worse or cause a heart attack. This is especially true for anti-clotting medicines (aspirin, clopidogrel, ticagrelor and prasugrel).
Your provider may recommend a cardiac rehabilitation program to help improve your heart's fitness.
SURGICAL TREATMENT
Some people will be able to control angina with medicines and not need surgery. Others will need a procedure called angioplasty and stent placement (also called percutaneous coronary intervention or PCI) to open blocked or narrowed arteries that supply blood to the heart.
Blockages that cannot be treated with angioplasty may need heart bypass surgery to redirect blood flow around the narrowed or blocked blood vessels.
Outlook (Prognosis)
Stable angina most often improves when taking medicines.
When to Contact a Medical Professional
Get medical help right away if you have new, unexplained chest pain or pressure. If you have had angina before, contact your provider.
Call 911 or the local emergency number if your angina pain:
- Is not better 5 minutes after you take nitroglycerin
- Does not go away after 3 doses of nitroglycerin
- Is getting worse
- Returns after the nitroglycerin helped at first
Contact your provider if:
- You are having angina symptoms more often
- You are having angina when you are sitting (rest angina)
- You are feeling tired more often
- You are feeling faint or lightheaded
- Your heart is beating very slowly (less than 60 beats a minute) or very fast (more than 120 beats a minute), or it is not steady (regular)
- You are having trouble taking your heart medicines
- You have any other unusual symptoms
Get medical help right away if a person with angina loses consciousness (passes out).
Prevention
Some studies have shown that making a few lifestyle changes can prevent blockages from getting worse and may actually improve them. Lifestyle changes can also help prevent some angina attacks. Your provider may tell you to:
- Lose weight if you are overweight
- Stop smoking
- Exercise regularly
- Drink alcohol in moderation only
- Eat a healthy diet that is high in vegetables, fruits, whole grains, fish, and lean meats
Your provider will also recommend that you keep other health conditions such as high blood pressure, diabetes, and high cholesterol levels under control.
If you have one or more risk factors for heart disease, talk to your provider about taking aspirin or other medicines to help prevent a heart attack. Aspirin therapy (75 to 325 mg a day) or medicines such as clopidogrel, ticagrelor or prasugrel may help prevent heart attacks in some people. Aspirin and other blood-thinning therapies are recommended if the benefit is likely to outweigh the risk of side effects.
Alternative Names
Angina - stable; Angina - chronic; Angina pectoris; Chest pain - angina; CAD - angina; Coronary artery disease - angina; Heart disease - angina
Images
References
Boden WE. Angina pectoris and stable ischemic heart disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 56.
Bonaca MP, Sabatine MS. Approach to the patient with chest pain. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 35.
Morrow DA, de Lemos J. Stable ischemic heart disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 40.
Virani SS, Newby LK, Arnold SV, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the management of patients with chronic coronary disease: A report of the American Heart Association/American College of Cardiology joint committee on clinical practice guidelines. Circulation. 2023;148(9):e9-e119. PMID: 37471501 pubmed.ncbi.nlm.nih.gov/37471501/.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19)2199-2269. PMID: 29146533 pubmed.ncbi.nlm.nih.gov/29146533/.
Writing Committee Members, Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;78(22):e187-e285. PMID: 34756653 pubmed.ncbi.nlm.nih.gov/34756653/.
Review Date 1/1/2025
Updated by: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.




