Angioplasty is a procedure to open narrowed or blocked blood vessels that supply blood to the heart. These blood vessels are called the coronary arteries.
A coronary artery stent is a small, metal mesh tube that expands inside a coronary artery. A stent is often placed during or immediately after angioplasty. It helps prevent the artery from closing up again. A drug-eluting stent has medicine embedded in it that helps prevent the artery from closing in the long term. These are the most common kind of stent.
 Watch this video about:Balloon angioplasty - short segment
Watch this video about:Balloon angioplasty - short segmentDescription
Before the angioplasty procedure begins, you will receive some pain medicine. You may also be given medicine that relaxes you, and blood-thinning medicines to prevent a blood clot from forming.
You will lie on a padded table. Your doctor (usually a heart specialist called a cardiologist) will insert a flexible tube (catheter) into an artery. Sometimes the catheter will be placed in your arm or wrist, or in your upper leg (groin) area. You will be awake during the procedure.
The doctor will use live x-ray pictures to carefully guide the catheter up into your heart and arteries. Liquid contrast (sometimes called "dye," will be injected into your body to highlight blood flow through the arteries. This helps the doctor see any blockages in the blood vessels that lead to your heart.
A guide wire is moved into and across the blockage. A balloon catheter is pushed over the guide wire and into the blockage. The balloon on the end is blown up (inflated). This opens the blocked vessel and restores proper blood flow to the heart.
A wire mesh tube (stent) may then be placed in this blocked area. The stent is inserted along with the balloon catheter. It expands when the balloon is inflated. The stent is left there to help keep the artery open.
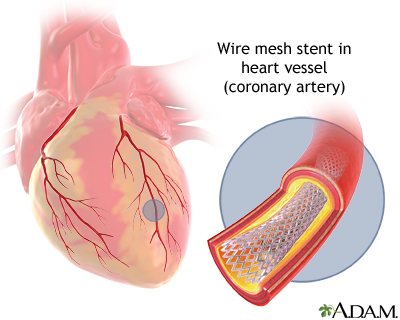
The stent is almost always coated with a drug (called a drug-eluting stent). This type of stent may lower the chance of the artery closing back up in the future.
Why the Procedure is Performed
Arteries can become narrowed or blocked by deposits called plaque. Plaque is made up of fat and cholesterol that builds up on the inside of artery walls. This condition is called hardening of the arteries (atherosclerosis).
Angioplasty may be used to treat:
- Blockage in a coronary artery during or after a heart attack
- Blockage or narrowing of one or more coronary arteries that may lead to poor heart function (heart failure)
- Narrowings that reduce blood flow and cause persistent chest pain (angina) that medicines do not control
Not every blockage can or needs to be treated with angioplasty. Some people who have several blockages or blockages in certain locations may need coronary bypass surgery. Some blockages are treated with medical therapy rather than an interventional procedure.
Risks
Angioplasty is generally safe, but ask your doctor about the possible complications. Risks of angioplasty and stent placement are:
- Allergic reaction to the drug used in a drug-eluting stent, the stent material (very rare), or the x-ray dye.
- Bleeding or clotting in the area where the catheter was inserted.
- Blood clot.
- Clogging of the inside of the stent (in-stent restenosis). This can be life threatening.
- Damage to a heart valve or blood vessel.
- Heart attack.
- Kidney failure (higher risk in people who already have kidney problems).
- Irregular heartbeat (arrhythmias).
- Stroke (this is rare).
Before the Procedure
Angioplasty is often performed when you go to the hospital or emergency room for chest pain, or after a heart attack. If you are admitted to the hospital for angioplasty:
- Tell your health care provider what medicines you are taking, even medicines or herbs you bought without a prescription.
- You will most often be asked not to drink or eat anything for 6 to 8 hours before the test.
- Take the mediciness your provider told you to take with a small sip of water.
- Tell your provider if you are allergic to seafood, you have had a bad reaction to contrast material or iodine in the past, you are taking sildenafil (Viagra) or similar medicines, or you are or might be pregnant.
After the Procedure
The average hospital stay is 2 days or less. Some people may not even have to stay overnight in the hospital.
In general, people who have angioplasty are able to walk around within a few hours after the procedure, depending on how the procedure went and where the catheter was placed. Complete recovery takes a week or less. You will be given information how to care for yourself after angioplasty.
Outlook (Prognosis)
For most people, angioplasty greatly improves blood flow through the coronary artery and the heart. It may help you avoid the need for coronary artery bypass surgery (CABG).
Angioplasty does not cure the cause of the blockage in your arteries. Your arteries may become narrow again.
Follow your heart-healthy diet, exercise, stop smoking (if you smoke), and reduce stress to lower your chances of having another blocked artery. Your provider may prescribe medicine to help lower your cholesterol or control your blood pressure. Taking these steps can help reduce your chances of complications from atherosclerosis.
Alternative Names
PCI; Percutaneous coronary intervention; Balloon angioplasty; Coronary angioplasty; Coronary artery angioplasty; Percutaneous transluminal coronary angioplasty; Heart artery dilatation; Angina - stent placement; Acute coronary syndrome - stent placement; Coronary artery disease - stent placement; CAD - stent placement; Coronary heart disease - stent placement; ACS - stent placement; Heart attack - stent placement; Myocardial infarction - stent placement; MI - stent placement; Coronary revascularization - stent placement
Images
References
Kumbhani DJ, Bhatt DL. Percutaneous coronary intervention. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 41.
Lawton, J, Tamis-Holland, JE. et al. 2021 ACC/AHA/SCAI Guideline for coronary artery revascularization: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;79(2):e21–e129. PMID: 34895950 pubmed.ncbi.nlm.nih.gov/34895950/.
Morrow DA, de Lemos J. Stable ischemic heart disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 40.
Virani SS, Newby LK, Arnold SV, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA guideline for the management of patients with chronic coronary disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. Circulation. 2023;148(9):e9–e119. PMID: 37471501 pubmed.ncbi.nlm.nih.gov/37471501/.
Review Date 7/14/2024
Updated by: Michael A. Chen, MD, PhD, Associate Professor of Medicine, Division of Cardiology, Harborview Medical Center, University of Washington Medical School, Seattle, WA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.



