A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack."
If blood flow is cut off for longer than a few seconds, the brain cannot get nutrients and oxygen. Brain cells can die, causing lasting damage.
A stroke can also occur if a blood vessel inside the brain bursts, leading to bleeding inside the head.
Causes
There are two major types of stroke:
- Ischemic stroke
- Hemorrhagic stroke
Ischemic stroke occurs when a blood vessel that supplies blood to the brain is blocked by a blood clot. This may happen in two ways:
- A clot may form in an artery that is already very narrow. This is called a thrombotic stroke.
- A clot may break off from another place in the blood vessels of the brain, or from some other part of the body, and travel up to the brain. This is called cerebral embolism, or an embolic stroke.
Ischemic strokes may also be caused by a sticky substance called plaque that can clog arteries.
 Watch this video about:Stroke
Watch this video about:StrokeA hemorrhagic stroke occurs when a blood vessel in part of the brain becomes weak and bursts open. This causes blood to leak into the brain. Some people have defects in the blood vessels of the brain that make this more likely. These defects may include:
- Aneurysm (weak area in the wall of a blood vessel that causes the blood vessel to bulge or balloon out)
- Arteriovenous malformation (AVM; abnormal connection between the arteries and veins)
- Cerebral amyloid angiopathy (CAA; condition in which proteins called amyloid build up on the walls of the arteries in the brain)
Hemorrhagic strokes may also occur when someone is taking blood thinners, such as dabigatran, rivaroxaban, apixaban, edoxaban and warfarin or has a bleeding disorder. Very high blood pressure may cause blood vessels to burst, leading to hemorrhagic stroke.
An ischemic stroke can develop bleeding and become a hemorrhagic stroke.
High blood pressure is the main risk factor for strokes. Other major risk factors are:
- Irregular heartbeat, called atrial fibrillation
- Diabetes
- Smoking
- Family history of stroke
- Being male
- High cholesterol
- Increasing age, especially after age 55
- Ethnicity (African Americans are more likely to die of a stroke)
- Obesity
- History of prior stroke or transient ischemic attack (occurs when blood flow to a part of the brain stops for a brief time)
Stroke risk is also higher in:
- People who have heart disease or poor blood flow in their legs caused by narrowed arteries
- People who have unhealthy lifestyle habits such as excessive use of alcohol, use of recreational drugs, a high-fat diet, or lack of exercise
- People who have a hereditary tendency to develop blood clots
- Women who take birth control pills (especially those who smoke and are older than 35)
- Women who are pregnant
- Women who take hormone replacement therapy
- Patent foramen ovale (PFO), a hole between the left and right atria (upper chambers) of the heart
- People who have sleep disorders (such as obstructive sleep apnea)
Symptoms
Symptoms of stroke depend on which part of the brain is damaged. In some cases, a person may not know that a stroke has occurred.
Most of the time, symptoms develop suddenly and without warning. But symptoms may occur on and off for the first day or two. Symptoms are usually most severe when the stroke first happens, but they may slowly get worse.
A headache may occur if the stroke is caused by bleeding in the brain. The headache:
- Starts suddenly and may be severe
- May be worse when you are lying flat
- May wake you up from sleep
- May get worse when you change positions or when you bend, strain, or cough
Other symptoms depend on how severe the stroke is, and what part of the brain is affected. Symptoms may include:
- Change in alertness (including sleepiness, unconsciousness, and coma)
- Changes in hearing or taste
- Changes that affect touch and the ability to feel pain, pressure, or different temperatures
- Confusion or loss of memory
- Problems swallowing
- Problems writing or reading
- Dizziness or abnormal feeling of movement (vertigo)
- Eyesight problems, such as decreased vision, double vision, or total loss of vision
- Lack of control over the bladder or bowels
- Loss of balance or coordination, or trouble walking
- Muscle weakness in the face, arm, or leg (usually just on one side)
- Numbness or tingling on one side of the body
- Personality, mood, or emotional changes
- Trouble speaking or understanding others who are speaking
Exams and Tests
Your health care provider will do a physical exam to:
- Check for problems with vision, movement, feeling, reflexes, understanding, and speaking. Your provider and nurses will repeat this exam over time to see if your stroke is getting worse or improving.
- Listen to the carotid arteries in the neck with a stethoscope for an abnormal sound, called a bruit, which is caused by abnormal blood flow.
- Check for high blood pressure and an irregular heartbeat.

You may have the following tests to help find the type, location, and cause of the stroke and check for other problems:
- CT scan or MRI scan of the brain to determine the location of the stroke, and if there is a mass, or any bleeding
- Angiogram of the head to look for a blood vessel that is blocked or bleeding
- Carotid duplex (ultrasound) to see if the carotid arteries in your neck have narrowed
- Echocardiogram to see if the stroke could have been caused by a blood clot from the heart
- Magnetic resonance angiography (MRA) or CT angiography to check for abnormal blood vessels in the brain
Other tests include:
- Blood tests
- Electroencephalogram (EEG) to determine if there are seizures
- Electrocardiogram (ECG) and heart rhythm monitoring
Treatment
A stroke is a medical emergency. Quick treatment is needed. Call 911 or the local emergency number right away or seek urgent medical care at the first signs of a stroke.
People who are having stroke symptoms need to get to a hospital as quickly as possible.
- If the stroke is caused by a blood clot, a clot-busting medicine may be given to dissolve the clot (also called thrombolytic therapy).
- To be effective, this treatment must be started within 4 1/2 hours of when the symptoms first started. However, the sooner this treatment is started, the better the chance of a good outcome.
- Endovascular thrombectomy may be needed. This is when a catheter is inserted into your arteries. Dye is injected while images of your brain's blood vessels are reviewed. A clot, if found, could be removed through the catheter.
Other treatments given in the hospital depend on the cause of the stroke. These may include:
- Blood thinners such as heparin, warfarin, direct acting oral anticoagulants (DOACs), aspirin, or clopidogrel (Plavix)
- Medicine to control risk factors for stroke, such as high blood pressure, diabetes, and high cholesterol
- Special procedures or surgery to relieve symptoms or prevent more strokes
- Nutrients and fluids
Physical therapy, occupational therapy, speech therapy, and swallowing therapy will all begin in the hospital. If the person has severe swallowing problems, a feeding tube in the stomach (gastrostomy tube) will likely be needed.
The goal of treatment after a stroke is to help you recover as much function as possible and prevent future strokes.
Recovery from your stroke will begin while you are still in the hospital or at a rehab center. It will continue when you go home from the hospital or center. Be sure to follow up with your provider after you go home.
Support Groups
More information and support for people with stroke and their families can be found on the American Stroke Association website -- www.stroke.org/en/help-and-support.
Outlook (Prognosis)
How well a person does after a stroke depends on:
- The type of stroke
- How much brain tissue is damaged
- What body functions have been affected
- How quickly treatment is given
Problems moving, thinking, and talking often start to improve in the days to weeks after a stroke.
Many people develop depression after a stroke. This can slow down recovery but is also a very treatable complication of a stroke.
Many people who have had a stroke will keep improving in the months or years after their stroke.
Over half of people who have a stroke are able to function and live at home. Others are not able to care for themselves.
If treatment with clot-busting medicines is successful, the symptoms of a stroke may go away. However, people often do not get to the hospital soon enough to receive these medicines, or they cannot take these medicines because of a health condition.
People who have a stroke from a blood clot (ischemic stroke) have a better chance of surviving than those who have a stroke from bleeding in the brain (hemorrhagic stroke).
The risk for a second stroke is highest during the weeks or months after the first stroke. The risk begins to decrease after this period.
When to Contact a Medical Professional
Stroke is a medical emergency that needs to be treated right away. The acronym F.A.S.T. is an easy way to remember signs of stroke and what to do if you think a stroke has occurred. The most important action to take is to call 911 or the local emergency number right away for emergency assistance.
F.A.S.T. stands for:
- FACE. Ask the person to smile. Check if one side of the face droops.
- ARMS. Ask the person to raise both arms. See if one arm drifts downward.
- SPEECH. Ask the person to repeat a simple sentence. Check if words are slurred and if the sentence is repeated correctly.
- TIME. If a person shows any of these symptoms, time is essential. It is important to get to the hospital as quickly as possible. Call 911 or the local emergency number. Act F.A.S.T.
Prevention
Reducing your stroke risk factors lessens your chance of having a stroke.
Alternative Names
Cerebrovascular disease; CVA; Cerebral infarction; Cerebral hemorrhage; Ischemic stroke; Stroke - ischemic; Cerebrovascular accident; Stroke - hemorrhagic; Carotid artery - stroke
Patient Instructions
- Angioplasty and stent placement - carotid artery - discharge
- Being active when you have heart disease
- Brain aneurysm repair - discharge
- Butter, margarine, and cooking oils
- Caring for muscle spasticity or spasms
- Carotid artery surgery - discharge
- Communicating with someone with aphasia
- Communicating with someone with dysarthria
- Constipation - self-care
- Dementia and driving
- Dementia - behavior and sleep problems
- Dementia - daily care
- Dementia - keeping safe in the home
- Dementia - what to ask your doctor
- Eating extra calories when sick - adults
- Headache - what to ask your doctor
- High blood pressure - what to ask your doctor
- Preventing falls
- Stroke - discharge
- Swallowing problems
Images
 Brain
Brain Carotid stenosis - X-ray of the left artery
Carotid stenosis - X-ray of the left artery Carotid stenosis - X-ray of the right artery
Carotid stenosis - X-ray of the right artery Stroke
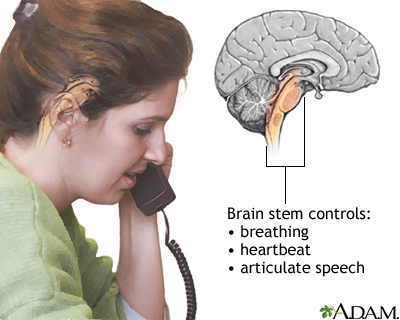
Stroke Brainstem function
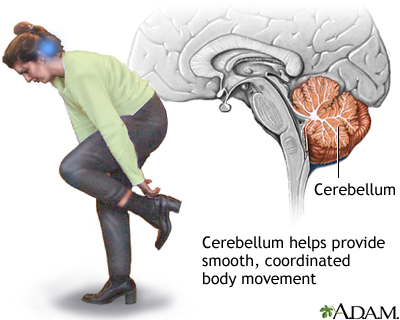
Brainstem function Cerebellum - function
Cerebellum - function Circle of Willis
Circle of Willis Left cerebral hemisphere - function
Left cerebral hemisphere - function Right cerebral hemisphere - function
Right cerebral hemisphere - function Endarterectomy
Endarterectomy Plaque buildup in arteries
Plaque buildup in arteries Stroke - series
Stroke - series Carotid dissection
Carotid dissection
References
Biller J, Schneck MJ, Ruland S. Ischemic cerebrovascular disease. In Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley's and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 65.
Bushnell C, Kernan WN, Sharrief AZ, et al. 2024 Guideline for the primary prevention of stroke: a guideline from the American Heart Association/American Stroke Association. Stroke. 2024;55(12):e344-e424. PMID: 39429201 pubmed.ncbi.nlm.nih.gov/39429201/.
Chaturvedi S, Selim M. Hemorrhagic cerebrovascular disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 377.
Gladstone DJ, Lindsay MP, Douketis J, et al. Canadian stroke consortium. Canadian stroke best practice recommendations: secondary prevention of stroke Update 2020. Can J Neurol Sci. 2022;49(3):315-337. PMID: 34140063 pubmed.ncbi.nlm.nih.gov/34140063/.
Goldstein LB. Ischemic cerebrovascular disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 376.
Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/AHA/ACCP/HRS Guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2024;149(1):e1-e156. PMID: 38033089 pubmed.ncbi.nlm.nih.gov/38033089/.
Kleindorfer DO, Towfighi A, Chaturvedi S, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021;52(7):e-364-e467. PMID: 34024117 pubmed.ncbi.nlm.nih.gov/34024117/.
Papa L, Meurer WJ. Stroke. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 87.
Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. PMID: 31662037 pubmed.ncbi.nlm.nih.gov/31662037/.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;72(3):e127-e248. PMID: 29133354 pubmed.ncbi.nlm.nih.gov/29133354/.
Review Date 4/16/2025
Updated by: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.















