Obesity means weighing more than what is healthy for a given height. Obesity is a serious, chronic disease. It can lead to other health problems, including diabetes, heart disease, and some cancers.
Causes
Taking in more calories than your body uses can lead to obesity. This is because your body stores unused calories as fat. Obesity can be caused by:
- Eating more food than your body can use
- Drinking too much alcohol
- Not getting enough exercise
Many people with obesity who lose large amounts of weight and gain it back think it is their fault. They blame themselves for not having the willpower to keep the weight off. Many people regain more weight than they lost.
Today, we know that biology is a big reason why some people cannot keep the weight off. Some people who live in the same place and eat the same foods develop obesity, while others do not. Our bodies have a complex system to keep our weight at a healthy level. In some people, this system does not work as well as it should.
The way we eat when we are children can affect the way we eat as adults.
The way we eat over many years becomes a habit. It affects what we eat, when we eat, and how much we eat.
We may feel that we are surrounded by things that make it easy to overeat and hard to stay active.
- Many people feel they do not have time to plan and make healthy meals.
- Many people do not have ready access to healthy foods making it difficult to plan and make healthy meals.
- More people today work desk jobs compared to more active jobs in the past.
- People with little free time may have less time to exercise.
The term eating disorder means a group of medical conditions that have an unhealthy focus on eating, dieting, losing or gaining weight, and body image. A person may have obesity, follow an unhealthy diet, and have an eating disorder all at the same time.
Sometimes, medical problems or treatments cause or contribute to weight gain, including:
- Underactive thyroid (hypothyroidism)
- Medicines such as birth control pills, antidepressants, and antipsychotics
Other things that can cause weight gain are:
- Quitting smoking -- Many people who quit smoking gain 4 to 10 pounds (lb) or 2 to 5 kilograms (kg) in the first 6 months after quitting.
- Stress, anxiety, feeling sad, depression, or not sleeping well.
- Menopause -- Women may gain 12 to 15 lb (5.5 to 7 kg) during menopause.
- Pregnancy -- Women may not lose the weight they gained during pregnancy.
Exams and Tests
Your health care provider will perform a physical exam and ask about your medical history, eating habits, and exercise routine.
The two most common ways to assess your weight and measure health risks related to your weight are:
- Body mass index (BMI)
- Waist circumference (your waist measurement in inches or centimeters)
BMI is calculated using height and weight. You and your provider can use your BMI to estimate how much body fat you have.
- Healthy weight is a BMI of 18.5 to 24.9 kg/m2
- Overweight is a BMI of 25.0 to 29.9 kg/m2
- Class 1 obesity is 30.0 to 34.9 kg/m2
- Class 2 obesity is 35.0 to 39.9 kg/m2
- Class 3 obesity is greater than or equal to 40.0 kg/m2
There are differences by race and ethnicity in the BMI value at which an increased risk for cardiometabolic abnormalities occurs. Your provider can help you apply this information to your own health risks.
For example, the BMI at which the risk of heart and other illnesses goes up is 25 kg/m2 in non-Hispanic Whites. The equivalent BMIs in other groups is:
- Non-Hispanic Blacks at a BMI of 22.9 kg/m2
- Hispanics at a BMI of 21.5 kg/m2
- South Asians at a BMI of 19.6 kg/m2
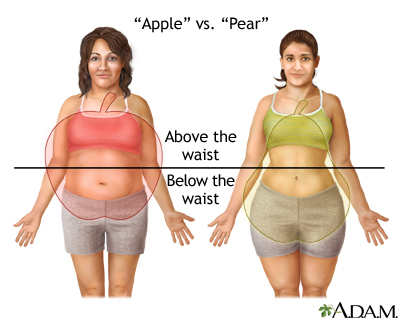
Your waist measurement is another way to estimate how much body fat you have. Extra weight around your middle or stomach area increases your risk for type 2 diabetes, heart disease, and stroke. People with "apple-shaped" bodies (meaning they tend to store fat around their waist and have a slim lower body) also have an increased risk for these diseases.
Body composition measures, including those that measure body fat, may be a more accurate tool than BMI for assessing obesity.
Treatment
CHANGING YOUR LIFESTYLE
An active lifestyle and plenty of exercise, along with healthy eating, is the safest way to lose weight. Even modest weight loss can improve your health. You may need a lot of support from family and friends.
Your main goal should be to learn new, healthy ways of eating and make them part of your daily routine.
Many people find it hard to change their eating habits and behaviors. You may have practiced some habits for so long that you may not even know they are unhealthy, or you do them without thinking. You need to be motivated to make lifestyle changes. Make the behavior change part of your life over the long term. Know that it takes time to make and keep a change in your lifestyle.
Work with your provider and dietitian to set realistic, safe daily calorie counts that help you lose weight while staying healthy. Remember that if you drop weight slowly and steadily, you are more likely to keep it off. Your dietitian can teach you about:
- Healthy food choices at home and in restaurants
- Healthy snacks
- Reading nutrition labels and healthy grocery shopping
- New ways to prepare food
- Portion sizes
- Sweetened drinks
Extreme diets (fewer than 1,100 calories per day) are not thought to be safe or to work very well. These types of diets often do not contain enough vitamins and minerals. Most people who lose weight this way return to overeating and develop obesity again.
Learn ways to manage stress other than snacking. Examples may be meditation, yoga, or exercise. If you are depressed or stressed a lot, talk to your provider.
MEDICINES AND HERBAL REMEDIES
You may see ads for supplements and herbal remedies that claim they will help you lose weight. Some of these claims may not be true. And some of these supplements can have serious side effects. Talk to your provider before using them.
You can discuss weight loss medicines with your provider. Many people lose at least 5 lb (2 kg) by taking these medicines, but they may regain the weight when they stop taking the medicine unless they have made lifestyle changes. Recently, some medicines called glucagon-like peptide-1 agonists (GLP-1 agonists) and another medicine called a dual glucose-dependent insulinotropic polypeptide and glucagon like peptide-1 receptor agonist have shown great promise to help people with obesity.
SURGERY
Weight-loss surgery (also called metabolic and bariatric surgery or MBS) can reduce the risk for certain diseases in people with severe obesity. These risks include:
- Arthritis
- Asthma
- Type 2 diabetes
- Gastroesophageal reflux disease (GERD)
- Heart disease
- High blood pressure
- Nonalcoholic fatty liver disease
- Obstructive sleep apnea
- Some cancers
- Stroke
Surgery may help people who have had obesity for 5 years or more and have not lost weight from other treatments, such as diet, exercise, or medicine.
Providers often use body mass index (BMI) and health conditions such as type 2 diabetes and high blood pressure to determine which people are most likely to benefit from MBS.
Surgery alone is not the answer for weight loss. It can train you to eat less, but you still have to do much of the work. You must be committed to diet, control portion sizes of what you eat, and exercise after surgery. Talk to your provider to learn if surgery is a good option for you.
Weight-loss surgeries include:
Support Groups
Many people find it easier to follow a diet and exercise program if they join a group of people with similar problems.
More information and support for people with obesity and their families can be found at:
Obesity Action Coalition -- www.obesityaction.org/education-support/tools/
Possible Complications
Obesity is a major health threat. The extra weight creates many risks to your health.
Alternative Names
Morbid obesity; Fat - obese
References
Barb D, Donahoo WT, Considine RV. Obesity: risk, risk factors, and medical management. In: Robertson RP, ed. DeGroot's Endocrinology. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 20.
Eisenberg D, Shikora SA, Aarts E, et al. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): Indications for Metabolic and Bariatric Surgery. Surg Obes Relat Dis. 2022;18(12):1345-1356. PMID: 36280539 pubmed.ncbi.nlm.nih.gov/36280539/.
Jastreboff AM, Kotz CM, Kahan S, Kelly AS, Heymsfield SB. Obesity as a disease: The Obesity Society 2018 position statement. Obesity (Silver Spring). 2019;27(1):7-9. PMID: 30569641 pubmed.ncbi.nlm.nih.gov/30569641/.
Jensen MD, Bessesen DH. Obesity. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 201.
Kirk S, Ogata B, Wichert E, Handu D, Rogza M. Treatment of pediatric overweight and obesity: position of the Academy of Nutrition and Dietetics based on an umbrella review of systematic reviews. J Acad Nutr Diet. 2022;122(4):848-861. PMID: 35063666 pubmed.ncbi.nlm.nih.gov/35063666/.
Raynor HA, Champagne CM. Position of the Academy of Nutrition and Dietetics: interventions for the treatment of overweight and obesity in adults. J Acad Nutr Diet. 2016;116(1):129-147. PMID: 26718656 pubmed.ncbi.nlm.nih.gov/26718656/.
Richards WO, Khaitan L, Torquati A. Morbid obesity. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St. Louis, MO: Elsevier; 2022:chap 48.
Shi Q, Wang Y, Hao Q, et al. Pharmacotherapy for adults with overweight and obesity: a systematic review and network meta-analysis of randomised controlled trials. Lancet. 2024;403(10434):e21-e31. 259-269. PMID: 38582569 pubmed.ncbi.nlm.nih.gov/38582569/.
Test Your Knowledge
Review Date 3/11/2024
Updated by: Frank D. Brodkey, MD, FCCM, Associate Professor, Section of Pulmonary and Critical Care Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.




