Abdominal pain is pain that you feel anywhere between your chest and groin. This is often referred to as the stomach region or belly.
Considerations
Almost everyone has pain in the abdomen at some point. Most of the time, it is not serious.
How bad your pain is does not always reflect the seriousness of the condition causing the pain.
For example, you might have very bad abdominal pain if you have gas or stomach cramps due to viral gastroenteritis.
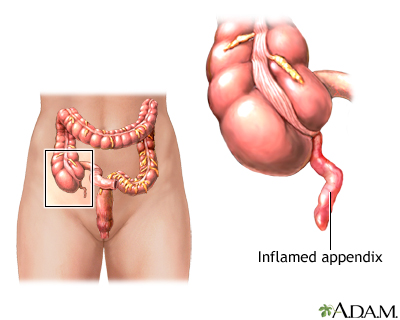
However, potentially fatal conditions, such as colon cancer or early appendicitis, may only cause mild pain or no pain.
Other ways to describe pain in your abdomen include:
- Generalized pain -- This means that you feel it in more than half of your belly. This type of pain is more typical for a stomach virus, indigestion, or gas. If the pain becomes more severe, it may be caused by a blockage of the intestines.
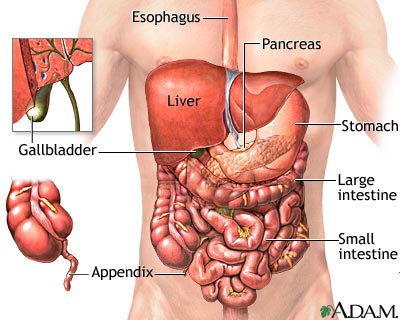
- Localized pain -- This is pain found in only one area of your belly. It is more likely to be a sign of a problem in an organ, such as the appendix, gallbladder, or stomach.
- Cramp-like pain -- This type of pain is not serious most of the time. It is likely to be due to gas and bloating, and is often followed by diarrhea. More worrisome signs include pain that occurs more often, lasts more than 24 hours, or occurs with a fever or rectal bleeding.
- Colicky pain -- This type of pain comes in waves. It very often starts and ends suddenly, and is often severe. Kidney stones and gallstones are common causes of this type of belly pain.
Causes
Many different conditions can cause abdominal pain. The key is to know when you need to get medical care right away. Sometimes, you may only need to contact a health care provider if your symptoms continue.
Less serious causes of abdominal pain include:
- Constipation
- Irritable bowel syndrome
- Food allergies or intolerance (such as lactose intolerance)
- Food poisoning
- Stomach flu
Other possible causes include:
- Appendicitis
- Abdominal aortic aneurysm (bulging and weakening of the major artery in the body)
- Bowel blockage or obstruction
- Cancer of the stomach, colon (large bowel), and other organs
- Cholecystitis (inflammation of the gallbladder) with or without gallstones
- Decreased blood supply to the intestines (ischemic bowel)
- Diverticulitis (inflammation and infection of the colon)
- Endometriosis
- Heartburn, indigestion, or gastroesophageal reflux (GERD)
- Hernia in which the intestine is stuck or twisted
- Inflammatory bowel disease (Crohn disease or ulcerative colitis)
- Kidney stones
- Muscle strain
- Pancreatitis (swelling or infection of the pancreas)
- Pelvic inflammatory disease (PID)
- Ruptured ovarian cyst
- Severe menstrual cramps
- Tubal (ectopic) pregnancy
- Ulcers
- Urinary tract infections (UTI)
Home Care
You can try the following home care steps to ease mild abdominal pain:
- Sip water or other clear fluids. You may have sports drinks in small amounts. People with diabetes must check their blood sugar often and adjust their medicines as needed.
- Avoid solid food for the first few hours.
- If you have been vomiting, wait 6 hours, and then eat small amounts of mild foods such as rice, applesauce, or crackers. Avoid dairy products.
- If the pain is high up in your abdomen and occurs after meals, antacids may help, especially if you feel heartburn or indigestion. Avoid citrus, high-fat foods, fried or greasy foods, tomato products, caffeine, alcohol, and carbonated beverages.
- DO NOT take any medicine without talking to your provider.
These additional steps may help prevent some types of abdominal pain:
- Drink plenty of water each day.
- Eat small meals more frequently.
- Exercise regularly.
- Limit foods that produce gas.
- Make sure that your meals are well-balanced and high in fiber. Eat plenty of fruits and vegetables.
When to Contact a Medical Professional
Get medical help right away or call 911 or the local emergency number if you:
- Are currently being treated for cancer
- Are unable to pass stool, especially if you are also vomiting
- Are vomiting blood or have blood in your stool (especially if bright red, maroon or dark, tarry black)
- Have chest, neck, or shoulder pain
- Have sudden, sharp abdominal pain
- Have pain in, or between, your shoulder blades with nausea
- Have tenderness in your belly, or your belly is rigid and hard to the touch
- Are pregnant or could be pregnant
- Had a recent injury to your abdomen
- Have difficulty breathing
Contact your provider if you have:
- Abdominal discomfort that lasts 1 week or longer
- Abdominal pain that does not improve in 24 to 48 hours, or becomes more severe and frequent and occurs with nausea and vomiting
- Bloating that persists for more than 2 days
- Burning sensation when you urinate or frequent urination
- Diarrhea for more than 5 days
- Fever, over 100°F (37.7°C) for adults or 100.4°F (38°C) for children, with pain
- Prolonged poor appetite
- Prolonged vaginal bleeding
- Unexplained weight loss
- Unable to keep down any foods or liquids
What to Expect at Your Office Visit
Your provider will perform a physical exam and ask about your symptoms and medical history. Your specific symptoms, the location of pain and when it occurs will help your provider detect the cause.
LOCATION OF YOUR PAIN
- Where do you feel the pain?
- Is it all over or in one spot?
- Does the pain move into your back, groin, or down your legs?
TYPE AND INTENSITY OF YOUR PAIN
- Is the pain severe, sharp, or cramping?
- Do you have it all the time, or does it come and go?
- Does the pain wake you up at night?
HISTORY OF YOUR PAIN
- Have you had similar pain in the past? How long has each episode lasted?
- When does the pain occur? For example, after meals or during menstruation?
- What makes the pain worse? For example, eating, stress, or lying down?
- What makes the pain better? For example, drinking milk, having a bowel movement, or taking an antacid?
- What medicines are you taking?
OTHER MEDICAL HISTORY
- Have you had a recent injury?
- Are you pregnant?
- What other symptoms do you have?
Tests that may be done include:
- Barium enema
- Blood, urine, and stool tests
- CT scan
- Colonoscopy or sigmoidoscopy (tube through the rectum into the colon)
- Electrocardiogram (ECG) or heart tracing
- Ultrasound of the abdomen
- Upper endoscopy (tube through the mouth into the esophagus, stomach and upper small intestine)
- Upper GI (gastrointestinal) and small bowel series
- X-rays of the abdomen
Alternative Names
Stomach pain; Pain - abdomen; Belly ache; Abdominal cramps; Bellyache; Stomachache
Patient Instructions
References
Landmann A, Bonds M, Postier R. Acute abdomen. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 46.
Martinez JP. Abdominal pain. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2018:chap 23.
McQuaid KR. Approach to the patient with gastrointestinal disease. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 118.
Weber F. Gastrointestinal and hepatic manifestations of systemic diseases. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 37.
Review Date 3/31/2024
Updated by: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.







