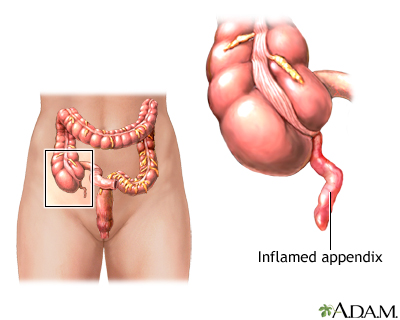
Appendicitis is a condition in which your appendix gets inflamed. The appendix is a small pouch attached to the end of the large intestine.
Causes
Appendicitis is a very common reason for emergency surgery. The problem most often occurs when the appendix becomes blocked by feces, a foreign object, a tumor or a parasite in rare cases.
Symptoms
The symptoms of appendicitis can vary. It can be hard to detect appendicitis in young children, older people, and women of childbearing age.
The first symptom is often pain around the belly button or mid upper abdomen. Pain may be minor at first, but becomes more sharp and severe. You may also have a loss of appetite, nausea, vomiting, and a low-grade fever.
The pain tends to move into the right lower part of your belly. The pain tends to focus at a spot directly above the appendix called McBurney point. This most often occurs 12 to 24 hours after the illness starts.
Your pain may be worse when you walk, cough, or make sudden movements. Later symptoms may include:
- Chills and shaking
- Diarrhea
- Fever
- Hard stools
- Nausea and vomiting
Exams and Tests
Your health care provider may suspect appendicitis based on the symptoms you describe.
Your provider will do a physical exam.
- If you have appendicitis, your pain will increase when your lower right belly area is pressed.
- If your appendix has ruptured, touching the belly area may cause a lot of pain and lead you to tighten your muscles.
- A rectal exam may find tenderness on the right side of your rectum.
A blood test will often show a high white blood cell count. Imaging tests that may help diagnose appendicitis include:
Treatment
Most of the time, a surgeon will remove your appendix as soon as you are diagnosed.
If a CT scan shows that you have an abscess, you may be treated with antibiotics first. You will have your appendix removed after the infection and swelling have gone away.
The tests used to diagnose appendicitis are not perfect. As a result, the operation may show that your appendix is normal. In that case, the surgeon will remove your appendix and explore the rest of your abdomen to check for other causes of your pain.
Outlook (Prognosis)
Most people recover quickly after surgery if the appendix is removed before it ruptures.
If your appendix ruptures before surgery, recovery may take longer. You are also more likely to develop problems, such as:
- An abscess
- Blockage of the intestine
- Infection inside the abdomen (peritonitis)
- Infection of the wound after surgery
When to Contact a Medical Professional
Contact your provider if you have pain in the lower-right portion of your belly, or other symptoms of appendicitis.
References
Carlberg DJ, Himelfarb NT. Acute appendicitis. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 79.
Expert Panel on Gastrointestinal Imaging:, Garcia EM, Camacho MA, et al. ACR appropriateness criteria right lower quadrant pain-suspected appendicitis. J Am Coll Radiol. 2018;15(11S):S373-S387. PMID: 30392606 pubmed.ncbi.nlm.nih.gov/30392606/.
Richmond B. The appendix. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 51.
Rosenthal MD, Sarosi GS. Appendicitis. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 120.
Sifri CD, Madoff LC. Appendicitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 78.
Review Date 4/21/2025
Updated by: Todd Eisner, MD, Private practice specializing in Gastroenterology in Boca Raton and Delray Beach, Florida at Gastroenterology Consultants of Boca Raton. Affiliate Assistant Professor, Florida Atlantic University School of Medicine. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.






