Venous insufficiency is a condition in which the veins have problems sending blood from the legs back to the heart.
Causes
Normally, valves in your deeper leg veins keep blood moving forward toward the heart. With long-term (chronic) venous insufficiency, vein walls are weakened and valves are damaged. This causes the veins to stay filled with blood, especially when you are standing.
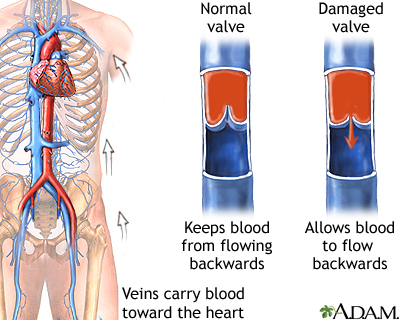
Chronic venous insufficiency is a long-term condition. It is most commonly due to malfunctioning (incompetent) valves in the veins. It may also occur as the result of a past blood clot in the legs.
Risk factors for venous insufficiency include:
- Age
- Family history of this condition
- Female sex (related to levels of the hormone progesterone)
- History of deep vein thrombosis in the legs
- Obesity
- Pregnancy
- Sitting or standing for long periods
- Tall height
Symptoms
Pain or other symptoms include:
- Dull aching, heaviness, or cramping in legs
- Itching and tingling
- Pain that gets worse when standing
- Pain that gets better when legs are raised
Skin changes in the legs include:
- Swelling of the legs
- Irritated or cracked skin if you scratch it
- Red or swollen, crusted, or weepy skin (stasis dermatitis)
- Varicose veins on the surface
- Thickening and hardening of the skin on the legs and ankles (lipodermatosclerosis)
- Wound or ulcer that is slow to heal on the legs or ankles
Exams and Tests
Your health care provider will do a physical exam and ask about your symptoms and medical history. Diagnosis is often made based on the appearance of leg veins when you are standing or sitting with your legs dangling.
A duplex ultrasound exam of your leg may be ordered to:
- Check how blood flows in the veins
- Check for other problems with the legs, such as a blood clot
Treatment
Your provider may suggest that you take the following self-care steps to help manage venous insufficiency:
- Do not sit or stand for long periods. Even moving your legs slightly helps keep the blood flowing.
- Care for wounds if you have any open sores or infections.
- Lose weight if you are overweight.
- Exercise regularly.
You can wear compression stockings to improve blood flow in your legs. Compression stockings gently squeeze your legs to move blood up your legs. This helps prevent leg swelling and, to a lesser extent, blood clots.
When more advanced skin changes are present, your provider:
- Should explain which skin care treatments can help, and which can make the problem worse
- May recommend some medicines that may help
Your provider may recommend more invasive treatments if you have:
- Leg pain, which may make your legs feel heavy or tired
- Skin sores caused by poor blood flow in the veins that do not heal or recur
- Thickening and hardening of the skin on the legs and ankles (lipodermatosclerosis)
Choices of procedures include:
- Sclerotherapy -- Salt water (saline), a chemical solution, or foam is injected into the vein. The vein hardens and then disappears.
- Phlebectomy -- Small surgical cuts (incisions) are made in the leg near the damaged vein. The vein is removed through one of the incisions.
- Procedures that can be done in a provider's office or clinic, such as using a laser, radiofrequency ablation, or a technique that uses a glue/foam to seal the vein.
- Varicose vein stripping -- Used to remove or tie off a large vein in the leg called the superficial saphenous vein.
Outlook (Prognosis)
Chronic venous insufficiency tends to get worse over time. However, it can be managed if treatment is started in the early stages. By taking self-care steps, you may be able to ease the discomfort and prevent the condition from getting worse. It is likely that you will need medical procedures to treat the condition.
When to Contact a Medical Professional
Contact your provider if:
- You have varicose veins and they are painful.
- Your condition gets worse or does not improve with self-care, such as wearing compression stockings or avoiding standing for too long.
- You have a sudden increase in leg pain or swelling, fever, redness of the leg, or leg sores.
Alternative Names
Chronic venous stasis; Chronic venous disease; Leg ulcer - venous insufficiency; Varicose veins - venous insufficiency
Images
References
Dalsing MC, Maleti O, Westin GG. Chronic venous insufficiency: deep vein valve reconstruction. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 159.
Markovic JN, Shortell CK. Treatment of chronic venous disorders. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 157.
Pascarella L, Marston W. Venous disease. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 21st ed. St Louis, MO: Elsevier; 2022:chap 65.
Review Date 5/10/2024
Updated by: Neil Grossman, MD, Saint Vincent Radiological Associates, Framingham, MA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.



