Mpox is a viral infection in which a person develops fever, fatigue, muscle aches, and a rash that may affect the entire body. Most cases resolve within 2 to 4 weeks.
This rare disease was regularly found mainly in central and western African countries. Since January 2023, there has been an ongoing outbreak in the Democratic Republic of Congo (DRC). The World Health Organization (WHO) recently declared this outbreak a Public Health Emergency of International Concern. This is the WHO's highest level of global alert, recognizing the potential threat to countries across the globe.
At this time, the Centers for Disease Control and Prevention has assessed the risk of infection to the general population in the United States as very low.
Causes
Mpox was first detected in Denmark in 1958 in a colony of monkeys used for research. This is how it first came to be called "monkeypox." The name was changed to mpox to reduce the stigma associated with the previous name. The first human case of mpox occurred in 1970 in the DRC.
In 2022, mpox spread to countries where mpox does not normally occur. This included countries in Europe, North and South America, the Middle East, and Australia.
Mpox is caused by Orthopoxvirus. It is similar to the virus that causes smallpox. There are two types of mpox virus: clade I and clade II.
- Clade I is endemic to Central Africa (including the DRC). Endemic means it is always present in some members of the population. Clade I is more severe and causes serious illness and death. It has killed as many as 10% of those infected. Recent death rates have been lower. Currently, there are no cases of Clade I mpox outside of central and eastern Africa.
- Clade II is endemic to West Africa. It is the type of mpox that caused the 2022 global outbreak. This type of mpox is much less severe, with nearly all people recovering from the illness. Clade II mpox is still spreading in small clusters in urban areas in the United States, but at much lower numbers than in 2022.
Both types of the Mpox virus are transmitted in the same way. Mpox can spread when a person comes into close contact with an infected animal, human, or material contaminated with the virus.
Mpox can be transmitted from animal to human when a person:
- Comes in contact with an infected animal
- Gets bitten or scratched by an infected animal
- Handles or consumes bushmeat
People with mpox can spread the virus to animals, such as pets and livestock.
Mpox can be transmitted from human to human through close contact, such as:
- Direct skin-to-skin contact with body fluids, sores, rash, or scabs from an infected person
- Touching objects, clothing, linens, or surfaces used by a person with mpox
- Exposure to large respiratory droplets
Mpox can be transmitted from human to human during intimate contact, including:
- Oral, anal, and vaginal sex
- Touching the genitals or anus of an infected person
- Hugging, kissing, cuddling, and massaging
- Face-to-face contact
- Touching fabrics or objects during sex that were used by a person with mpox such as bedding, towels, and sex toys
A pregnant woman can spread the virus to their fetus through the placenta.
Symptoms
Symptoms usually appear in 1 to 3 weeks after exposure to the virus.
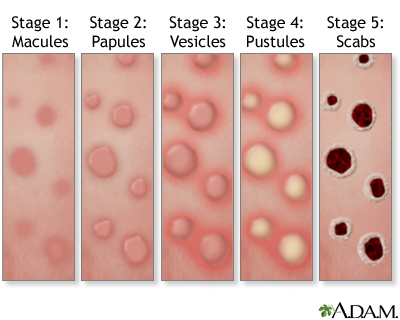
A rash appears that can be found on or near the genitals and can appear on all parts of the body. The rash starts as flat spots that become raised bumps, which fill with fluid, then pus. The bumps may be painful. Soon they crust over and form itchy scabs that fall off and heal over.
Flu-like symptoms include:
You may experience all or just some of the symptoms.
- You may have flu-like symptoms followed by the rash in 1 to 4 days
- You may get the rash first, then the flu-like symptoms
- Or you may just have a rash
Some people can spread the virus anywhere from 1 to 4 days before having any symptoms.
Mpox illness lasts about 2 to 4 weeks. You are no longer contagious only after:
- All symptoms are gone
- Scabs have healed completely
- New skin has formed
Exams and Tests
Your health care provider can diagnose mpox by looking at the rash and asking questions about your medical history.
Your provider may take specimens from your skin lesions and send them for testing. A PCR test (polymerase chain reaction test) can confirm the diagnosis.
Treatment
Currently, there is no specific treatment for the mpox virus. In most people, symptoms usually go on their own in 2 to 4 weeks.
Certain people may be at risk for more severe disease and may need to be hospitalized and given supportive care:
- People with severe symptoms
- People whose immune system is not working well
- Women who are pregnant or breastfeeding
- Children younger than 8 years old
Antivirals used for smallpox may be helpful in treating mpox in people who are more likely to get severely ill.
Home care for mpox can help prevent the spread and keep you more comfortable.
- Do not pop or scratch the lesions and do not shave the area.
- Avoid touching the rash, as you can spread it to other parts of the body.
- Cover lesions with bandages or gauze to help prevent spreading the virus.
- Try over-the-counter (OTC) topical products such as benzocaine/lidocaine for pain and calamine lotion or petroleum jelly for itching.
- OTC oral antihistamines may also help with itching.
- An oatmeal bath may help with itching. Using a sitz bath or sitting in shallow water in the tub can help with lesions on the genitals. Epsom salt, vinegar, or baking soda can be added to the water to help soothe the area.
- Keep the area dry and clean (except when washing).
- Wash your hands often with soap and water or sanitizer, especially after touching the rash.
- For a rash on your hands, wear comfortable gloves when touching surfaces or objects in shared spaces.
- Wear a well-fitting face mask around other people until all of your symptoms are gone and your skin is healed.
- OTC pain relievers such as ibuprofen (Advil, Motrin) and acetaminophen (Tylenol) can help relieve pain. Your provider may prescribe something stronger, if needed.
Outlook (Prognosis)
In most people, symptoms go away within 2 to 4 weeks. Rarely, severe cases may lead to death.
When to Contact a Medical Professional
Contact your provider if you:
- Think you may have been exposed to mpox
- Develop symptoms of mpox
- Have an unexplained rash
If you have mpox, you should contact your provider if:
- Your symptoms do not improve
- The rash becomes infected
- You have nausea, vomiting, diarrhea, or dehydration
- The rash spreads to your eyes, mouth, genitals, or anus
Prevention
The Centers for Disease Control and Prevention (CDC) recommends vaccination for people at risk for mpox:
- People who have had known or suspected contact with someone with mpox
- People who have had sex with someone in the past two weeks who was diagnosed with mpox
- People with multiple sexual partners in an area where mpox is spreading
- Men who have sex with anyone who has had a recent sexually transmitted infection in the last 6 months
- People in jobs that may expose them to the virus, such as those who work in health care, public health, or clinical or research laboratory workers
- People who have sex with a partner who is at risk for mpox infection
The CDC also recommends vaccination if you are traveling to a country with a clade I mpox outbreak and may engage in any the following activities during travel:
- Sex with a new partner
- Sex at a sex club, bathhouse, or other commercial sex venue
- Sex in exchange for money, goods, drugs, or other trade
- Sex at a rave, party, festival, or other large public event
If you have mpox, remember that you can still spread the virus until skin lesions heal completely and all symptoms are gone. To help prevent infecting others:
- Stay away from other people until you heal completely (isolate at home).
- If you live with other people, stay in one room away from others.
- Disinfect commonly used surfaces after each use, such as in the bathroom or kitchen.
- Cover all shared furniture with sheets or blankets.
- Wear a well-fitting mask when around other people and pets in your household.
- Do not share items you have touched with others.
- Avoid contact with pets and other animals.
The CDC has more information on disinfecting your home to protect others.
For more information on the current outbreak:
- Centers for Disease Control and Prevention: Clade I Mpox Outbreak Originating in Central Africa -www.cdc.gov/monkeypox/outbreaks/2023/index.html
- World Health Organization: Mpox (monkeypox) - www.who.int/health-topics/mpox#tab=tab_1
Alternative Names
Poxvirus; Orthopoxvirus; Monkeypox
Images
References
Centers for Disease Control and Prevention website. Clinical features of monkeypox. www.cdc.gov/monkeypox/hcp/clinical-signs/. Updated September 12, 2024. Accessed October 15, 2025.
Centers for Disease Control and Prevention website. Clinical treatment of monkeypox. www.cdc.gov/monkeypox/hcp/clinical-care/. Updated August 29, 2025. Accessed October 15, 2025.
Centers for Disease Control and Prevention website. How monkeypox spreads. www.cdc.gov/monkeypox/causes/. Updated January 30, 2025. Accessed October 15, 2025.
Centers for Disease Control and Prevention website. Monkeypox in the United States and around the world: current situation. www.cdc.gov/monkeypox/situation-summary/index.html. Updated September 15, 2025. Accessed October 15, 2025.
Centers for Disease Control and Prevention website. Monkeypox vaccination. www.cdc.gov/monkeypox/vaccines/index.html. Updated September 15, 2025. Accessed October 15, 2025.
Centers for Disease Control and Prevention website. What to do if you are sick. www.cdc.gov/monkeypox/caring/. Updated August 5, 2025. Accessed October 15, 2025.
Centers for Disease Control and Prevention website. Preventing monkeypox. www.cdc.gov/monkeypox/prevention/. Updated December 11, 2024. Accessed October 15, 2025.
Centers for Disease Control and Prevention website. Signs and symptoms of monkeypox. www.cdc.gov/monkeypox/signs-symptoms/. Updated September 12, 2024. Accessed October 15, 2025.
Review Date 8/29/2024
Updated by: Jatin M. Vyas, MD, PhD, Roy and Diana Vagelos Professor in Medicine, Columbia University Vagelos College of Physicians and Surgeons, Division of Infectious Diseases, Department of Medicine, New York, NY. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team. Editorial update 02/05/2025.



