Acute bronchitis is swelling and inflamed tissue in the bronchi, the main passages that carry air to the lungs. This swelling narrows the airways, which makes it harder to breathe. Other symptoms of bronchitis are a cough and coughing up mucus. Acute means the symptoms have been present only for a short time.
Causes
When acute bronchitis occurs, it almost always comes after having a cold or flu-like illness. The bronchitis infection is usually caused by a virus. At first, it affects your nose, sinuses, and throat. Then it spreads to the airways that lead to your lungs.
Sometimes, bacteria also infect your airways. This is more common in people with chronic obstructive pulmonary disease chronic obstructive pulmonary disease (COPD).
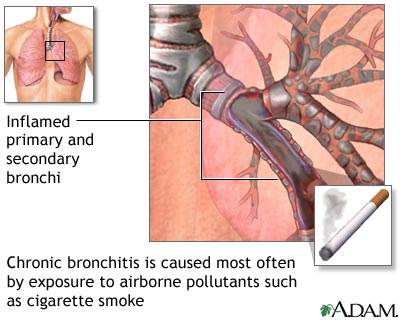
Chronic bronchitis is a long-term condition. To be diagnosed with chronic bronchitis, you must have a cough with mucus on most days for at least 3 months.
Symptoms
Some symptoms of acute bronchitis are:
- Chest discomfort
- Cough that produces mucus -- the mucus may be clear or yellow-green
- Fatigue
- Fever -- usually low-grade
- Shortness of breath that gets worse with activity
- Wheezing, in people with asthma
Even after acute bronchitis has cleared, you may have a dry, nagging cough that lasts for 1 to 4 weeks.
Sometimes it can be hard to know if you have pneumonia or bronchitis. If you have pneumonia, you are more likely to have a high fever and chills, feel sicker, or feel more short of breath.
Exams and Tests
Your health care provider will listen to the breathing sounds in your lungs with a stethoscope. Your breathing may sound abnormal or rough.
Tests may include:
- Chest x-ray, if your provider suspects pneumonia
- Pulse oximetry, a painless test that helps determine the amount of oxygen in your blood by using a device placed on the end of your finger

Treatment
Most people DO NOT need antibiotics for acute bronchitis caused by a virus. The infection will almost always go away on its own within 1 week, though a mild cough may persist for up to 3 weeks. Doing these things may help you feel better:
- Drink plenty of fluids.
- If you have asthma or another chronic lung condition, use your inhaler.
- Get plenty of rest.
- Take aspirin or acetaminophen if you have a fever. DO NOT give aspirin to people under age 18.
- Breathe moist air by using a humidifier or steaming up the bathroom.
Certain medicines that you can buy without a prescription can help break up or loosen mucus. Look for the word "guaifenesin" on the label. If needed, ask the pharmacist for help finding it.
If your symptoms do not improve or if you are wheezing, your provider may prescribe an inhaler to open your airways.
If your provider thinks you also have bacteria in your airways, they may prescribe antibiotics. This medicine will only get rid of bacteria, not viruses.
Your provider may also prescribe corticosteroid medicine to reduce swelling in your lungs.
If you have influenza and it is caught in the first 48 hours after getting sick, your provider might also prescribe antiviral medicine.
Other tips include:
- DO NOT smoke.
- Avoid secondhand smoke and air pollution.
- Wash your hands (and your children's hands) often to avoid spreading viruses and other germs.
Outlook (Prognosis)
Except for the cough, symptoms usually go away in 7 to 10 days if you do not have a lung disorder. Coughing often lasts for 2 to 3 weeks.
When to Contact a Medical Professional
Contact your provider if you:
- Have a cough on most days, or have a cough that keeps returning
- Are coughing up blood
- Have a high fever or shaking chills
- Have a low-grade fever for 3 or more days
- Have thick, yellow-green mucus, especially if it has a bad smell
- Feel short of breath or have chest pain
- Have a chronic illness, like heart or lung disease
Patient Instructions
References
Bearman GM, Wenzel RP. Acute bronchitis and tracheitis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 84.
Centers for Disease Control and Prevention website. Acute bronchitis. Chest cold (acute bronchitis) basics. www.cdc.gov/acute-bronchitis/about/. Updated April 17, 2024. Accessed June 18, 2024.
Cherry JD. Acute bronchitis. In: Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ, eds. Feigin and Cherry's Textbook Of Pediatric Infectious Diseases. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 19.
Walsh EE. Acute bronchitis. In: Bennett JE, Dolin R, Blaser MJ, eds. Mandell, Douglas and Bennett's Principles and Practice of Infectious Diseases. 9th ed. Philadelphia, PA: Elsevier; 2020:chap 65.
Review Date 2/3/2024
Updated by: Frank D. Brodkey, MD, FCCM, Associate Professor, Section of Pulmonary and Critical Care Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.









