Rheumatoid arthritis (RA) is a disease that leads to inflammation of the joints and surrounding tissues. It is a long-term disease. It can also affect other organs.
Causes
The cause of RA is not known. It is an autoimmune disease. This means the immune system of the body mistakenly attacks healthy tissue.
RA can occur at any age, but is more common in middle age. Women get RA more often than men.
Infection, genes, and hormone changes may be linked to RA. Smoking and the gut microbiome are linked to the risk of developing the disease.
It is less common than osteoarthritis (OA) which is a joint condition that occurs in many people due to wear and tear on the joints as they age.
Symptoms
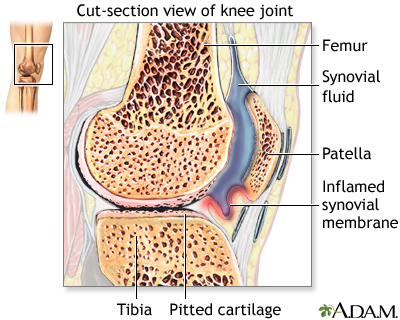
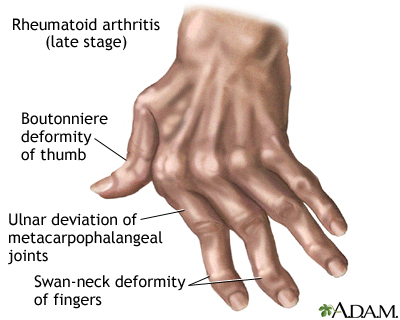
Most of the time, RA affects joints on both sides of the body equally. Fingers, wrists, knees, feet, elbows, ankles, hips and shoulders are the most commonly affected. The lower spine is usually not affected by RA.
The disease often begins slowly. Early symptoms may include:
- Minor joint pain
- Stiffness
- Fatigue
Joint symptoms may include:
- Morning stiffness, which lasts more than 1 hour, is common.
- Joints may feel warm, tender, and stiff when not used for an hour.
- Joint pain is often felt in the same joint on both sides of the body.
- Joints are often swollen.
- Over time, joints may lose their range of motion and may become deformed.
Other symptoms include:
- Chest pain when taking a breath (pleurisy)
- Dry eyes and mouth (Sjögren syndrome)
- Eye burning, itching, and discharge
- Nodules under the skin (most often a sign of more severe disease)
- Numbness, tingling, or burning in the hands and feet
- Sleep difficulties
The diagnosis of RA is made when:
- You have pain and swelling in 1 or more joints.
- Pain and swelling have been present for longer than 6 weeks.
- You have a positive test for rheumatoid factor or anti-cyclic citrullinated peptide (anti-CCP) antibody.
- You have an elevated erythrocytesedimentation rate (ESR) or C-reactive protein (CRP) levels.
- Other types of arthritis are not present.
Sometimes the diagnosis of RA is made even without all of the conditions shown above if the arthritis is otherwise typical for RA.
Exams and Tests
There is no test that can determine for sure whether you have RA. Most people with RA will have some abnormal test results. However, some people will have normal results for all tests.
Two lab tests that are positive in most people and often help in the diagnosis are:
- Rheumatoid factor
- Anti-CCP antibody
These tests are positive in most patients with RA. The anti-CCP antibody test is more specific for RA.
Other tests that may be done include:
- Complete blood count (CBC)
- Metabolic panel and serum uric acid
- CRP
- ESR
- Antinuclear antibody
- Tests for hepatitis
- Joint x-rays
- Joint ultrasound or MRI
- Joint fluid analysis
Treatment
RA most often requires long-term treatment by an expert in arthritis called a rheumatologist. Treatment includes:
- Medicines
- Physical therapy
- Exercise
- Education to help you understand the nature of RA, your treatment options, and the need for regular follow-up
- Surgery, if required
Early treatment for RA with medicines called disease-modifying antirheumatic drugs (DMARDs) should be used in all patients. This will slow joint destruction and prevent deformities. The activity of the RA should be checked at regular visits to make sure the disease is under control. The goal of treatment is to stop the progression of the RA.
MEDICINES
Anti-inflammatory medicines: These include aspirin and nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, naproxen and celecoxib.
- These medicines work very well to reduce joint swelling and inflammation, but they can have long-term side effects. Therefore, they should be taken only for a short time and in low doses when possible.
- Since they do not prevent joint damage if used alone, DMARDs should be used as well.
Disease modifying antirheumatic drugs (DMARDs): These are often the medicines that are tried first in people with RA. They are prescribed along with rest, strengthening exercise, and anti-inflammatory drugs.
- Methotrexate is the most commonly used DMARD for RA. Leflunomide and hydroxychloroquine may also be used.
- Sulfasalazine is a medicine that is often combined with methotrexate and hydroxychloroquine (triple therapy).
- It may be weeks or months before you see any benefit from these medicines.
- These medicines may have serious side effects, so you will need frequent blood tests and other monitoring when taking them.
- Antimalarial medicines -- This group of medicines includes hydroxychloroquine (Plaquenil). They are most often used along with methotrexate. It may be weeks or months before you see any benefit from these medicines.
Corticosteroids -- These medicines work very well to reduce joint swelling and inflammation, but they can have long-term side effects and do not prevent joint damage if used alone. Therefore, they should be taken only for a short time and in low doses when possible.
Biologic DMARD agents -- These medicines are designed to affect parts of the immune system that play a role in the disease process of RA.
- They may be given when other medicines, usually methotrexate, have not worked. Biologic medicines are often added to methotrexate. However, because they are very expensive, insurance approval is generally required.
- Most of them are given either under the skin or into a vein. There are now many different types of biologic agents.
Biologic and synthetic agents can be very helpful in treating RA. However, people taking these medicines must be watched closely because of uncommon, but serious adverse reactions:
- Infections from bacteria, viruses, and fungi
- Skin cancer, but not melanoma
- Skin reactions
- Allergic reactions
- Worsened heart failure
- Damage to nerves
- Low white blood cell count
SURGERY
Surgery may be needed to correct severely damaged joints. Surgery may include:
- Removal of the joint lining (synovectomy)
- Total joint replacement, in extreme cases, may include total knee replacement or total hip replacement.
PHYSICAL THERAPY
Range-of-motion exercises and exercise programs prescribed by a physical therapist can delay the loss of joint function and help keep muscles strong.
Sometimes, therapists will use special machines to apply deep heat or electrical stimulation to reduce pain and improve joint movement.
Other therapies that may help ease joint pain include:
- Joint protection techniques
- Heat and cold treatments
- Splints or orthotic devices to support and align joints
- Frequent rest periods between activities, as well as 8 to 10 hours of sleep per night
NUTRITION
Some people with RA may have intolerance or allergies to certain foods. A balanced nutritious diet is recommended. It may be helpful to eat foods rich in fish oils (omega-3 fatty acids). Smoking cigarettes should be stopped. Excessive alcohol should also be avoided.
Support Groups
More information and support for people with RA and their families can be found by taking part in an arthritis support group.
Some people may benefit from taking part in an arthritis support group.
Outlook (Prognosis)
Whether your RA progresses or not depends on the severity of your symptoms and your response to treatment. It is important to start the treatment as soon as possible. Regular follow up visits with a rheumatologist are needed to adjust the treatment.
Permanent joint damage may occur without proper treatment. Early treatment with a three-medicine DMARD combination known as "triple therapy," or with biologic or targeted synthetic medicines can prevent joint pain and damage.
Possible Complications
If not well treated, RA can affect nearly every part of the body. Complications may include:
- Damage to the lung tissue.
- Increased risk of hardening of the arteries, leading to cardiovascular disease.
- Spinal injury when the neck bones become damaged.
- Inflammation of the blood vessels (rheumatoid vasculitis), which can lead to skin, nerve, heart, and brain problems.
- Swelling and inflammation of the outer lining of the heart (pericarditis) and of the heart muscle (myocarditis), which can lead to congestive heart failure.
However, these complications can be avoided with proper treatment. The treatments for RA can also cause serious side effects. Talk to your provider about the possible side effects of treatment and what to do if they occur.
When to Contact a Medical Professional
Contact your provider if you think you have symptoms of rheumatoid arthritis.
Prevention
There is no known prevention. Smoking appears to worsen RA, so it is important to avoid tobacco. Proper early treatment can help prevent further joint damage.
Alternative Names
RA; Arthritis - rheumatoid
Patient Instructions
References
England BR, O'Dell JR. Treatment of rheumatoid arthritis. In: Firestein GS, McInnes IB, Koretzky GA, Mikuls TR, Neogi T, O'Dell JR, eds. Firestein & Kelley's Textbook of Rheumatology. 12th ed. Philadelphia, PA: Elsevier; 2025:chap 73.
Fraenkel L, Bathon JM, England BR, et al. 2021 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken). 2021;73(7):924-939. PMID: 34101387 pubmed.ncbi.nlm.nih.gov/34101387/.
McInnes IB. Rheumatoid arthritis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 243.
Test Your Knowledge
Review Date 1/28/2025
Updated by: Diane M. Horowitz, MD, Rheumatology and Internal Medicine, Northwell Health, Great Neck, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.





