Hepatitis B is irritation and swelling (inflammation) of the liver due to infection with the hepatitis B virus (HBV).
Other types of viral hepatitis include hepatitis A, hepatitis C, hepatitis D, and hepatitis E.
Causes
You can catch hepatitis B infection through contact with the blood or body fluids (semen, vaginal fluids, and saliva) of a person who has the virus.
Exposure may occur:
- After a needlestick or sharps injury
- If any blood or other body fluid touches your skin, eyes or mouth, or open sores or cuts
People who may be at risk for hepatitis B are those who:
- Have unprotected sex with an infected partner
- Receive blood transfusions (not common in the United States)
- Have contact with blood at work (such as health care workers)
- Have been on long-term kidney dialysis
- Get a tattoo or acupuncture with unclean needles
- Share needles or straws during drug use
- Share personal items (such as toothbrush, razor, and nail clippers) with a person who has the virus
- Were born to a hepatitis-B infected mother
All blood used for blood transfusions is screened, so the chance of getting the virus in this way is very small.
Symptoms
After you first become infected with the HBV:
- You may have no symptoms.
- You may feel sick for a period of days or weeks.
- You may become very ill very quickly (called fulminant hepatitis).
Symptoms of hepatitis B may not appear for up to 6 months after the time of infection. Early symptoms include:
- Appetite loss
- Fatigue
- Low fever
- Muscle and joint aches
- Nausea and vomiting
- Yellow skin and dark urine
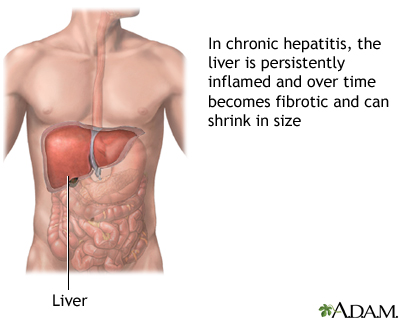
Symptoms will go away in a few weeks to months if your body is able to fight off the infection. Some people never get rid of the HBV. This is called chronic hepatitis B.
People with chronic hepatitis may not have symptoms and may not know they are infected. Over time, they may develop symptoms of liver damage and cirrhosis of the liver.
You can spread the HBV to other people, even if you have no symptoms.
Exams and Tests
A series of blood tests, called the hepatitis viral panel, is done for suspected hepatitis. It can help detect:
- New infection
- Older infection that is still active
- Older infection that is no longer active
The following tests are done to look for liver damage if you have chronic hepatitis B:
- Albumin level.
- Liver function tests.
- Prothrombin time.
- Other blood tests may be used to assess how much liver scarring you have.
You may also have a test to measure the level of HBV in your blood (viral load). This lets your health care provider know how your treatment is working.
Imaging tests, such as ultrasound, MRI, and others are also often recommended.
SCREENING
The CDC recommends that all adults over age 18 be screened for Hepatitis B. This may be needed even when they have no symptoms. Factors that lead to increased risk include:
- The risk factors described above in the Causes section.
- People from countries where a higher number of people have hepatitis B. These countries or areas include Japan, some Mediterranean countries, parts of Asia and the Middle East, West Africa, and South Sudan.
Treatment
Acute hepatitis, unless severe, needs no treatment. Liver and other body functions are watched using blood tests. You should get plenty of rest, drink plenty of fluids, and eat healthy foods.
Some people with chronic hepatitis B may be treated with antiviral drugs. These medicines can decrease or remove hepatitis B from the blood. Examples include pills such as tenofovir (Viread), entecavir (Baraclude), and lamivudine (Epivir) or an injection called interferon. They also help to reduce the risk for cirrhosis and liver cancer.
It is not always clear which people with chronic hepatitis B should receive drug therapy and when it should be started. You are more likely to receive these medicines if:
- Your liver function is quickly becoming worse.
- You develop symptoms of long-term liver damage.
- You have high levels of the HBV in your blood.
- You are pregnant.
For these medicines to work best, you need to take them as instructed by your provider. Ask what side effects you can expect and what to do if you have them. Not everybody who takes these medicines responds well.
If you develop liver failure, you may be considered for a liver transplant. A liver transplant is the only cure in some cases of liver failure.
Other steps you can take:
- Avoid alcohol.
- Check with your provider before taking any over-the-counter medicines or herbal supplements. This includes medicines such as acetaminophen, aspirin, or ibuprofen.
Severe liver damage or cirrhosis can be caused by hepatitis B.
Support Groups
More information and support for people with HBV condition and their families can be found by joining a support group. Ask your provider about liver disease resources and support groups in your area.
Outlook (Prognosis)
The acute illness most often goes away after 2 to 3 weeks. The liver returns to normal within 4 to 6 months in most people.
Almost all newborns and about one half of children who get hepatitis B develop the chronic condition. Very few adults who get the virus develop chronic hepatitis B.
A newborn born to a mother with hepatitis B is given hepatitis B immune globulin (HBIG).
There is a much higher rate of liver cancer in people who have chronic hepatitis B. For this reason, people with Hepatitis B are screened for liver cancer.
When to Contact a Medical Professional
Contact your provider if:
- You develop symptoms of hepatitis B.
- Your hepatitis B symptoms do not go away in 2 to 3 weeks, or new symptoms develop.
- You belong to a high-risk group for hepatitis B and have not had the HBV vaccine.
Prevention
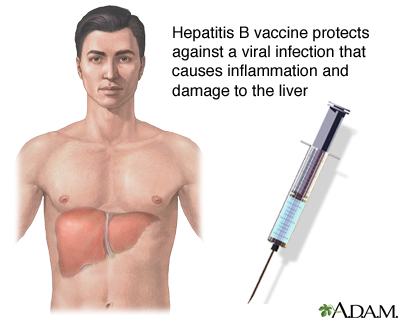
The best way to prevent hepatitis B is to get the vaccine. The CDC recommends that children and adults get the hepatitis vaccine.
Children and people at high risk for hepatitis B should get the hepatitis B vaccine.
- Babies should get a first dose of the hepatitis B vaccine at birth. They should have all 3 shots in the series by age 6 to 18 months.
- Children younger than age 19 years who have not had the vaccine should get "catch-up" doses.
- Health care workers and those who live with someone who has hepatitis B should get the vaccine.
- Infants born to mothers who have acute hepatitis B or have had the infection in the past should get a special hepatitis B vaccine within 12 hours of birth.
The hepatitis B vaccine or a hepatitis B immune globulin (HBIG) shot may help prevent infection if you receive it within 24 hours of contact with the virus.
Measures to avoid contact with blood and body fluids can help prevent the spread of hepatitis B from person-to-person.
References
Centers for Disease Control and Prevention website. Adult Immunization Schedule by Age (Addendum updated June 27, 2024). www.cdc.gov/vaccines/hcp/imz-schedules/adult-age.html. November 16, 2023. Accessed September 5, 2024.
Centers for Disease Control and Prevention website. Vaccine Schedules for You and Your Family. Updated February 10, 2023. Accessed September 5, 2024. www.cdc.gov/vaccines/imz-schedules/index.html.
Conners EE, Panagiotakopoulos L, Hofmeister MG, et al. Screening and Testing for Hepatitis B Virus Infection: CDC Recommendations - United States, 2023. MMWR Recomm Rep. 2023 Mar 10;72(1):1-25. PMID: 36893044. pubmed.ncbi.nlm.nih.gov/36893044/.
Janssen HLA, Fung S. Hepatitis B. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 79.
Pawlotsky J-M. Acute viral hepatitis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 134.
Pawlotsky J-M. Chronic viral and autoimmune hepatitis. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 135.
Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH; American Association for the Study of Liver Diseases. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63(1):261-283. PMID: 26566064 pubmed.ncbi.nlm.nih.gov/26566064/.
Review Date 3/31/2024
Updated by: Jenifer K. Lehrer, MD, Department of Gastroenterology, Aria - Jefferson Health Torresdale, Jefferson Digestive Diseases Network, Philadelphia, PA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.






