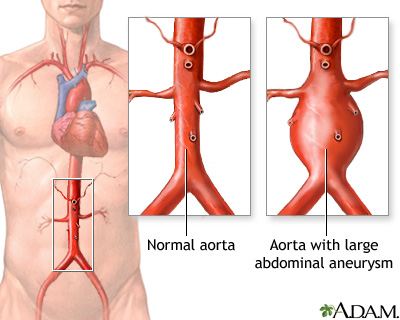
The aorta is the main blood vessel that supplies blood to the abdomen, pelvis, and legs. An abdominal aortic aneurysm (AAA) occurs when an area of the aorta in the abdomen becomes very large or balloons out.
Causes
The exact cause of an aneurysm is unknown. It occurs due to weakness in the wall of the artery. Factors that can increase your risk of having this problem include:
- Smoking
- High blood pressure
- Male sex
- Genetic factors
An abdominal aortic aneurysm is most often seen in males over age 60 who have one or more risk factors. The larger the aneurysm, the more likely it is to break open or tear. This can be life threatening.
Symptoms
Aneurysms can develop slowly over many years, often with no symptoms. Symptoms may come on quickly if the aneurysm expands rapidly, tears open or leaks blood within the wall of the vessel (aortic dissection).
Symptoms of rupture include:
- Pain in the abdomen or back. The pain may be severe, sudden, persistent, or constant. It may spread to the groin, buttocks, or legs.
- Passing out.
- Clammy skin.
- Dizziness.
- Nausea and vomiting.
- Rapid heart rate.
- Shock.
Exams and Tests
Your health care provider will examine your abdomen and feel the pulses in your legs. The provider may find:
- A lump (mass) in the abdomen
- Pulsating sensation in the abdomen
- Stiff or rigid abdomen
Your provider may find this problem by doing the following tests:
- Ultrasound of the abdomen when the abdominal aneurysm is first suspected
- CT scan of the abdomen to confirm the size of the aneurysm
- CTA (computed tomographic angiogram) to help with surgical planning
Any one of these tests may be done when you are having symptoms.
You may have an abdominal aortic aneurysm that is not causing any symptoms. Your provider may order an ultrasound of the abdomen to screen for an aneurysm.
- Most men who are age 65 to 75, who have smoked during their life should have this test one time.
- Some men who are age 65 to 75, who have never smoked during their life may need this test one time.
Treatment
If you have bleeding inside your body from an aortic aneurysm, you will need surgery right away.
If the aneurysm is small and there are no symptoms:
- Surgery is rarely done.
- You and your provider must decide if the risk of having surgery is smaller than the risk of bleeding if you do not have surgery.
- Your provider will want to check the size of the aneurysm with ultrasound tests. The recommended frequency depends on the size of your aneurysm. Ask your provider what is best for you.
Most of the time, surgery is done if the aneurysm is bigger than 2 inches (5 centimeters) across or growing quickly. The goal is to do surgery before complications develop.
There are two types of surgery:
- Open repair - A large cut is made in your abdomen. The abnormal vessel is replaced with a graft made of man-made material.
- Endovascular stent grafting - This procedure can be done without making a large cut in your abdomen, so you may recover more quickly. This may be a safer approach if you have certain other medical problems or are an older adult. Endovascular repair can sometimes be done for a leaking or bleeding aneurysm.
Outlook (Prognosis)
The outcome is often good if you have surgery to repair the aneurysm before it ruptures.
When an abdominal aortic aneurysm begins to tear or ruptures, it is a medical emergency. Only about 1 in 5 people survive a ruptured abdominal aneurysm.
When to Contact a Medical Professional
Go to the emergency room or call 911 or the local emergency number if you have pain in your belly or back that is very bad or does not go away.
Prevention
To reduce the risk of aneurysms:
- Eat a heart-healthy diet, exercise, stop smoking (if you smoke), and reduce stress.
- If you have high blood pressure or diabetes, take your medicines as your provider has told you.
People over age 65 who have ever smoked should have a screening ultrasound done once.
Alternative Names
Aneurysm - aortic; AAA
References
Braverman AC, Schermerhorn M. Diseases of the aorta. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 42.
Colwell CB. Abdominal aortic aneurysm. In: Walls RM, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 72.
Isselbacher EM, Preventza O, Black JH 3rd, et al. 2022 ACC/AHA Guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022;80(24) e223–e393. PMID: 36334952 pubmed.ncbi.nlm.nih.gov/36334952/.
Owens DK, Davidson KW, Krist AH, et al. Screening for abdominal aortic aneurysm: US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322(22):2211-2218. PMID: 31821437 pubmed.ncbi.nlm.nih.gov/31821437/.
Sharafuddin MJ. Abdominal aortic aneurysms: open surgical treatment. In: Sidawy AN, Perler BA, eds. Rutherford's Vascular Surgery and Endovascular Therapy. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 73.
Review Date 8/22/2023
Updated by: Mary C. Mancini, MD, PhD, Cardiothoracic Surgeon, Shreveport, LA. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.




