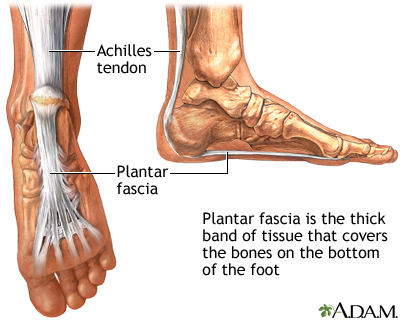
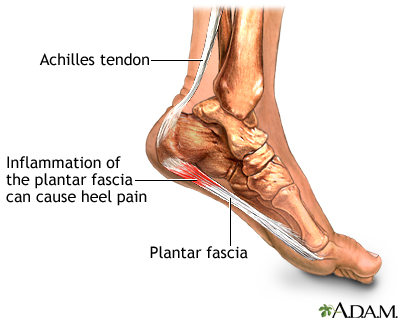
The plantar fascia is the thick tissue on the bottom of the foot. It connects the heel bone to the toes and creates the arch of the foot. When this tissue becomes swollen or inflamed, it is called plantar fasciitis.
Causes
Swelling occurs when the thick band of tissue on the bottom of the foot (fascia) is overstretched or overused. This can be painful and make walking more difficult.
You are more likely to get plantar fasciitis if you:
- Have foot arch problems (both flat feet and high arches)
- Run long distances, downhill or on uneven surfaces
- Are obese or gain weight suddenly
- Have a tight Achilles tendon (the tendon connecting the calf muscles to the heel)
- Wear shoes with poor arch support or soft soles
- Change your activity level
Plantar fasciitis is seen in both men and women. It is one of the most common orthopedic foot complaints.
Plantar fasciitis was commonly thought to be caused by a heel spur. However, research has found that this is not the case. On x-ray, heel spurs are seen in people with and without plantar fasciitis.
Symptoms
The most common symptom is pain and stiffness in the bottom of the heel. The heel pain may be dull or sharp. The bottom of the foot may also ache or burn.
The pain is often worse:
- In the morning when you take your first steps
- After standing or sitting for awhile
- When climbing stairs
- After intense activity
- During walking, running, and jumping sports
The pain may develop slowly over time, or come on suddenly after intense activity.
Exams and Tests
The health care provider will perform a physical exam. This may show:
- Pain and tenderness on the bottom of your foot
- Pain and tenderness along the sole of the foot
- Flat feet or high arches
- Mild foot swelling or redness
- Stiffness or tightness of the arch in the bottom of your foot
- Stiffness or tightness with your Achilles tendon or calf muscles
X-rays may be taken to check for other problems.
Treatment
Your provider will often recommend these steps first:
- Acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) to reduce pain and inflammation.
- Physical therapy with emphasis on heel and foot stretching exercises.
- Night splints to wear while sleeping to stretch the foot.
- Resting as much as possible for at least a week.
- Wearing shoes with good support and cushions.
You can also apply ice to the painful area. Do this at least twice a day for 10 to 15 minutes, more often in the first couple of days.
If these treatments do not work, your provider may recommend:
- Wearing a boot cast, which looks like a ski boot, for 3 to 6 weeks. It can be removed for bathing.
- Custom-made shoe inserts (orthotics).
- Steroid shots or injections into the heel.
Sometimes, foot surgery is needed.
Outlook (Prognosis)
Nonsurgical treatments almost always improve the pain. Treatment can last from several months to 2 years before symptoms get better. Most people feel better within 6 to 18 months. Rarely, surgery may be needed to relieve the pain.
When to Contact a Medical Professional
Contact your provider if you have symptoms of plantar fasciitis.
Prevention
Making sure your ankle, Achilles tendon, and calf muscles are flexible can help prevent plantar fasciitis. Stretch your plantar fascia in the morning before you get out of bed. Doing activities in moderation can also help.
Images
References
Grear BJ. Disorders of tendons and fascia and adolescent and adult pes planus. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 83.
Kadakia AR, Aiyer AA. Heel pain and plantar fasciitis: hindfoot conditions. In: Miller MD, Thompson SR, eds. DeLee, Drez, & Miller's Orthopaedic Sports Medicine. 5th ed. Philadelphia, PA: Elsevier; 2020:chap 120.
McGee DL. Podiatric procedures. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges' Clinical Procedures in Emergency Medicine and Acute Care. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 51.
Review Date 6/17/2024
Updated by: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.




